Dry eye syndrome, or keratoconjunctivitis sicca, is a common multifactorial condition affecting millions of people every year. Symptoms may include irritated eyes, a gritty or sandy feeling, burning, a foreign body sensation, blurry vision, or excess watering. Increased osmolarity of the tear film and ocular surface inflammation and damage can result.
Normal Anatomy and Physiology
Lubrication of your eyes involves the lacrimal glands, ocular surface (cornea and conjunctiva), eyelids, meibomian glands, goblet cells in the conjunctiva, and associated sensory and motor nerves.
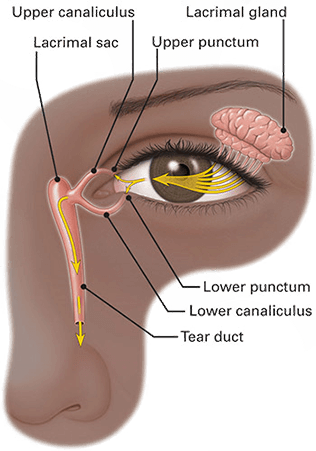
Blinking spreads the tear film over the ocular surface toward the medial canthus (the inner corner of the eye). There the tears drain into the superior and inferior punctae (one punctum in each eyelid) and enter the lacrimal canaliculi. The canaliculi converge into a common canaliculus which conveys tears to the lacrimal sac. Then tears travel down the nasolacrimal duct, which empties into the nose.
The tear film consists of three components: an inner mucin layer close to the cornea (window of the eye) for even spreading, a middle water layer with moisture and proteins for resistance to infection, and an outer oil (lipid) layer to seal the tear film.
The mucous component or the innermost layer of the tear film contains mucins which are produced by goblet cells in the conjunctiva (the thin, clear membrane that covers the front surface of the white portion of the eye) and stratified squamous cells of the cornea (the circular, clear, front surface of the eye) and conjunctiva. The mucous layer lubricates the ocular surface, provides a sticky interface between the hydrophobic ocular surface epithelium and the aqueous layer, and traps foreign particles, cellular debris, and microbes which, with blinking, are moved to the medial canthus where they exit the eye.
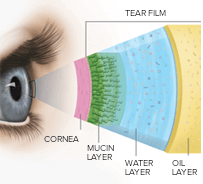
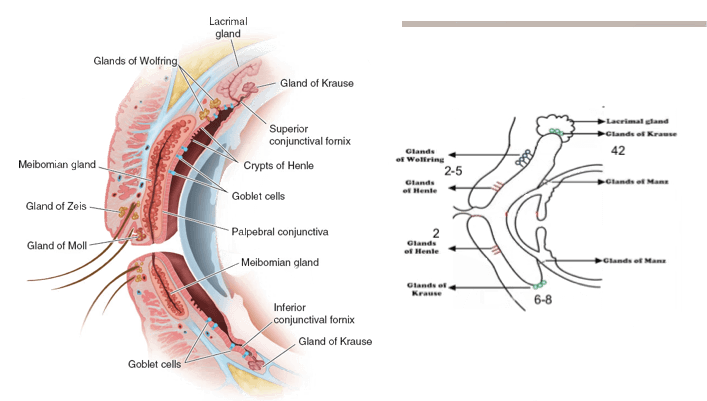
The aqueous component, the main portion of the tear film, lies on top of (or in front of) the mucous layer. It is produced by the lacrimal glands, which include: (1) the main lacrimal gland (located in the superior temporal region of the orbit) and its palpebral lobe (extending into the upper eyelid), and (2) the accessory lacrimal glands of Krause and Wolfring.
The aqueous component includes water and electrolytes; antibacterial proteins such as lysozyme, lactoferrin, and immunoglobulins (especially IgA); vitamins, particularly vitamin A (also known as retinol, which is required for corneal maintenance); and growth factors (epidermal growth factor and hepatocyte growth factor). The aqueous layer hydrates the mucous layer; supplies oxygen and electrolytes to the ocular surface; provides antibacterial defense; maintains and renews the ocular surface; and promotes wound healing.
The lipid component covers the aqueous layer and is the outermost layer of the tear film. It is produced by the meibomian glands, located in the tarsal plates of the eyelids, which open onto the lid margin just behind the eyelashes. There is also a small contribution from the glands of Zeis, which open into the eyelash follicles.
The lipid layer slows tear evaporation, enhances tear film spreading, provides a smooth optical surface, prevents contamination of the tear film by skin lipids, retards overflow of tears (in the absence of excessive reflex tearing), and seals the lid margins during sleep.
Causes, Aggravators, And Associated Conditions
AQUEOUS DEFICIENCY
Non-Sjogren’s Syndrome
- Lacrimal Deficiency
- Ex. After radiation involving the area of the lacrimal gland
- Obstruction of Lacrimal Gland Duct
- Reflex Block-Corneal insensitivity-Neurotrophic cornea
- Neurotrophic cornea-Caused by damage to the trigeminal (5th cranial) nerve
- Previous LASIK
- Systemic conditions
- Ex. Rheumatoid arthritis (adversely affects lacrimal glands and reduces tear secretion), lupus
- Systemic Medications
- Ex. Antihistamines, diuretics, beta-blockers, antispasmodics, some psychotropics
- Aging
Sjogren’s Syndrome
- Primary – Occurs without another underlying rheumatologic disorder
- Secondary – Associated with another autoimmune disease, such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), or scleroderma
EVAPORATION
Intrinsic
- Meibomian Oil (from glands in lids) Deficiency in Blepharitis and Meibomitis
- Systemic Conditions
- Rosacea adverses affects meibomian gland dysfunction and causes inflammation
- Disorders of Lid Aperature or Position
- Ex. Graves or thyroid eye disease, ectropion (sagging of the lower lid away from the eye) previous blepharoplasties, Bell’s palsy caused by malfunction of the facial (7th cranial) nerve (if the affected eye cannot adequately close), syndromes which affect the patient’s lid position or ability to close the lid(s) such as Goldenhar (with a lid coloboma or notch), Treacher Collins, Moebius, Stevens-Johnson
- Low Blink Rate
- Ex. Parkinson’s disease or looking at electronics too long without blinking
- Drug Action
- Ex. Accutane, chemotherapy
Extrinsic
- Vitamin A Deficiency
- Topical Drugs
- Ex. Antihistamine eye drops for allergies, preservatives in eye drops
- Contact Lens Wear
- Ocular Surface Disease
- Ex. Allergies
- Environment
- Ex. Live in the desert, work in a casino or other building with high ventilation, use of fans
Treatments
Conservative-Medical
- Artificial tears (with and without tear evaporation protection), liquigel/gel drops, gel, ointment
- Dry eyes are most often first addressed with daily use of ocular lubricants such as artificial tears, gel drops, gel, or lubricating ointment
- Popular brands-Refresh/Systane/GenTeal/Thera Tears/Optive
- Treating blepharitis and meibomitis, eyelid conditions which characteristically have deficient secretion of oil from the meibomian glands, can yield significant relief of dry eyes.
- Re-esterified omega-3 fatty acids in fish oil or flaxseed oil supplements (1-3g two to three times daily by mouth per day) help retard the evaporation of tears because omega-3 fatty acids soften lipids in the meibomian glands of the eyelids and improve their release of lipids to the outer tear film layer.
- Warm compresses/dry rice in a sock or silk sac/hard-boiled egg without the shell wrapped in a paper towel/warm water in a balloon
- Derm masks/Heated eye pad (heatedeyepad.com)
- Lid hygiene-Blephadex wipes
- Prescription medications (please see below)
- Treatments with medical devices such as BlephEx, IPL, Lipiflow, and iLux (please see below)
- Avoiding blowing fans in the room while sleeping or redirecting a ceiling fan to blow air upward instead of downward
- Wearing an eye mask while sleeping to prevent dessicating drafts from fans, to hold moisture over your eyes, or to hinder pressurized air from a CPAP or biPAP from reaching your eyes
- Eyeseals 4.0 Hydrating Sleep Mask (eyeeco)-shield eyes from air from CPAP machines, drafts, low humidity
- Tranquileyes goggles (eyeeco)-with memory foam inserts to hold moisture/liquid
- Adding a humidifier to your home
Prescription Medications
- Restasis – Lubricates and reduces inflammation
- Xiidra – Lubricates and reduces inflammation
- Cequa – Lubricates and reduces inflammation
- Erythromycin/bacitracin ophthalmic ointment
- Doxycycline/clarithromycin/azithromycin
- Topical steroids, if there is an inflammatory component
Minimally-Invasive Medical Intervention
- Punctal plugs-semipermanent silicone punctal plugs
- Intracanicular plugs-synthetic 6-month dissolvable plugs placed in the upper and/or lower canaliculus(i)
- Punctal occlusion by cautery
- Lacrisert-sterile, slow release pellet/lubricant (hydroxypropyl cellulose) placed in the inferior fornix (performed by patients)
- Bandage contact lenses
- Amniotic membrane graft, e.g. BioDOptix amniotic membrane can be placed on the eye with an overlying bandage contact lens for ocular tissue repair
Medical Treatments-In Office

- BlephEx®- BlephEx® is a painless procedure that removes scurf and collarettes, particulate matter (similar to dandruff) along the edge of your eyelids and eyelashes, using a rotating soft medical-grade microsponge.
- Lipiflow and iLux are automated thermal pulsation treatments that address meibomian gland dysfunction with heat and massage.
- IPL with manual meibomian gland expression-Intense Pulsed Light-pulses of light which liquify and improve the flow of meibomian gland oil to improve gland function and dry eyes. Also reduces inflammation and vascularization of the eyelids, brown/age spots, and rosacea.

Lumenis M22 IPL (Intense Pulse Light)
In addition to the BlephEx, Dr. Shin also has the Lumenis M22 IPL to help improve your meibomian gland function and your dry eyes. With meibum (meibomian gland oil) that is thicker than usual, the meibomian glands of many patients do not secrete oil to the tear film properly. Inflammation and bacterial overgrowth compound the problem. Standard treatments include warm compresses (for other forms of applied heat, please see above under conservative treatments) to try to melt the meibum, lid scrubs to cleanse the lid margin and lower the bacterial load, and topical antibiotic/anti-inflammatory medications and oral antibiotics to decrease associated inflammation. IPL produces photobiomodulation (a process that stimulates cell mitochondria and promotes healthy cell function,) so it serves as an effective adjunct to chronic treatments.
The Lumenis M22 IPL delivers intense pulses of non-coherent xenon flashlamp light in wavelengths of 400nm to 1200nm through a continuously-cooled applicator. To address meibomian gland function, a 560nm filter is used to allow passage of wavelengths of light above 560nm and below 1200nm to be applied through a 15mm by 35 mm continuously-cooled applicator to your gel-covered skin below the lower eyelid and/or orbital bones while you wear eye shields. This is followed by manual meibomian gland expression by Dr. Shin. Other IPL settings are chosen for maximal safety with attention to your Fitzpatrick skin type and optimal efficacy.
These 10-15 minute treatments heat the meibum, close abnormal blood vessels which have been secreting inflammatory mediators, and eradicate bacteria, which brings relief to dry, red, sore, and irritated eyes. Therefore, IPL can be especially helpful for rosacea and acne patients. Patients generally receive the best results with four treatment sessions three to four weeks apart followed by maintenance applications every six to 12 months. Patients treated for meibomian gland dysfunction may notice rejuvenated skin in the treated area because IPL also stimulates collagen and elastic fiber production; reduces pigmentation, age/sun spots and broken capillaries; and improves overall skin appearance. IPL can be applied to other areas of the face for photorejuvenation.
Technology to Help Qualify and Determine the Severity of Dry Eye Disease
Antares

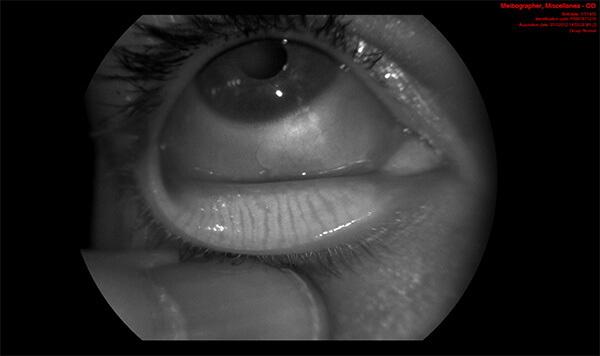
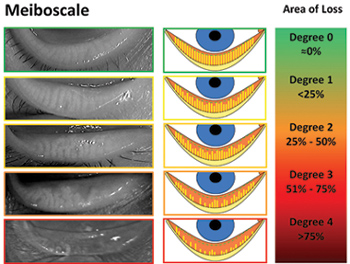
Besides traditional examination methods, Dr. Shin incorporates the Antares to further analyze your dry eyes. This noninvasive state-of-the-art device provides advanced tear film analysis by dynamically measuring the break-up time of your tears, using fluoroscopy to measure tear break-up time, determining your tear meniscus height, and displaying a dynamic video map of the surface curvature of your cornea. Because aberrations in the corneal surface can affect your refractive error and your vision, Dr. Shin interprets the color-coded images to help treat patients with eye refracting issues. Importantly, as meibomian gland dysfunction is the leading cause of evaporative dry eye, the Antares also analyzes and classifies meibomian gland function through lipid layer grading and infrared meibography.
Call our offices and schedule a consultation with our Las Vegas Ophthalmologist, Dr. Shin, today.








